In 2019, the Department of Health and Human Services’ Office of Inspector General (HHS OIG) released a report listing several “significant vulnerabilities” in hospice care provided to Medicare beneficiaries. The report offered an overview of hospice care deficiencies around the country.
Life-threatening deficiencies were identified in hundreds of facilities nationwide. Unsanitary conditions, failure to detect sexual misconduct, and untreated wounds were some of the most shocking shortcomings mentioned in the report.
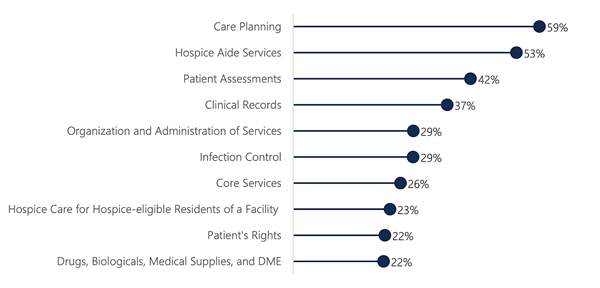
The most frequently observed deficiencies in hospice care facilities Source: HHS OIG
In 2017, Medicare paid $17.8 billion for hospice care provided to nearly 1.5 million patients. The report has shown that over 300 out of a total of 4,563 facilities providing hospice care for Medicare beneficiaries are poor performers. In New York, 93 percent of the facilities surveyed were found to have at least one deficiency. Following the study’s release, the HHS OIG’s Assistant Inspector General, Erin Bliss, said that the numbers are “unacceptable” and that substandard care is actually harming patients.
Some of the most shocking cases referenced in the report included:
- A patient whose leg had to be amputated due to an untreated wound
- Maggots found around a feeding tube
- Staff that failed to recognize signs of sexual abuse
- A patient who had a wound that went untreated for two years
- Staff that moved a patient in an unsafe way, resulting in a fall and a broken leg
Main Findings of the Inspector General’s Report on Hospice Care Deficiencies
Titled “Hospice Deficiencies Pose Risks to Medicare Beneficiaries,” the report concluded that the majority of the hospices surveyed had at least one care deficiency, and called for action to protect beneficiaries. After reviewing complaint reports from 2012 through 2016, researchers presented statistical data about 50 serious deficiencies, concluding that:
- More than 80 percent of hospices had at least one deficiency
- 20 percent of hospices had at least one serious deficiency
- Common deficiencies included inadequate care planning, mismanagement of aide services, poor assessment of beneficiaries, improperly vetting staff, and insufficient quality control
- Complaints were filed against over 30 percent of hospices
- Approximately 15 percent had severe complaints filed against them
- Over 300 active hospices are poor performers
Inspector General’s Recommendations to Improve Hospice Care and Protect Beneficiaries
The Inspector General made a series of recommendations to remedy this critical situation:
- Expand deficiency data reporting requirements
- Include this information on Hospice Compare
- Educate hospices about common deficiencies that put residents at risk
- Carefully monitor compliance by hospices with a track record of severe deficiencies
In another HHS OIG report, titled “Safeguards Must Be Strengthened to Protect Medicare Hospice Beneficiaries from Harm,” researchers stated that Medicare hospice beneficiaries are frequently harmed due to poor care, abuse by caregivers, and hospices failing to take action against abuse and neglect. “Hospices did not face serious consequences for the harm described in this report,” the analysts wrote.
According to a spokesperson for the National Partnership for Hospice Innovation, which represents not-for-profit hospices all over the U.S., the government must “increase oversight on hospice programs...that cause serious harm to patients and their families."
Today, the only way to protect patients from harm and stop misconduct is to file a False Claims Act (“FCA”) lawsuit with the help of a whistleblower attorney. Under the FCA, Medicare fraud whistleblowers who file a complaint resulting in monetary recoveries can receive between 10 and 30 percent of the recovered taxpayer funds.